Written by Mr Sachin Malde for Doctify
Incontinence is not exactly a common topic of conversation. Some people might relegate it as a term that applies only to the elderly. However, with stress incontinence, this is not the case. This condition affects a range of different people and it should be talked about with more openness and no feelings of shame.
Here to educate us on the realities of stress incontinence is Urologist, Mr Sachin Malde.
What is stress urinary incontinence?
Stress urinary incontinence is leakage of urine when you increase the pressure on your bladder, such as by laughing, coughing, sneezing or exercising. It is the most common type of incontinence in women and it affects one in five women over the age of 40.
What causes stress urinary incontinence?
Stress urinary incontinence occurs when the pelvic floor muscles that support the bladder are weakened. This commonly happens as a result of childbirth but a number of other factors can increase the chances of stress urinary incontinence:
- Increasing age
- Overweight
- Multiple vaginal deliveries
- Post-menopausal
- In men after prostate operations
How can stress urinary incontinence be treated?
As a specialist in the treatment of stress urinary incontinence, I regularly see women with different degrees of incontinence, and so the treatment options vary depending on how severe your symptoms are.
Are there any non-surgical treatments?
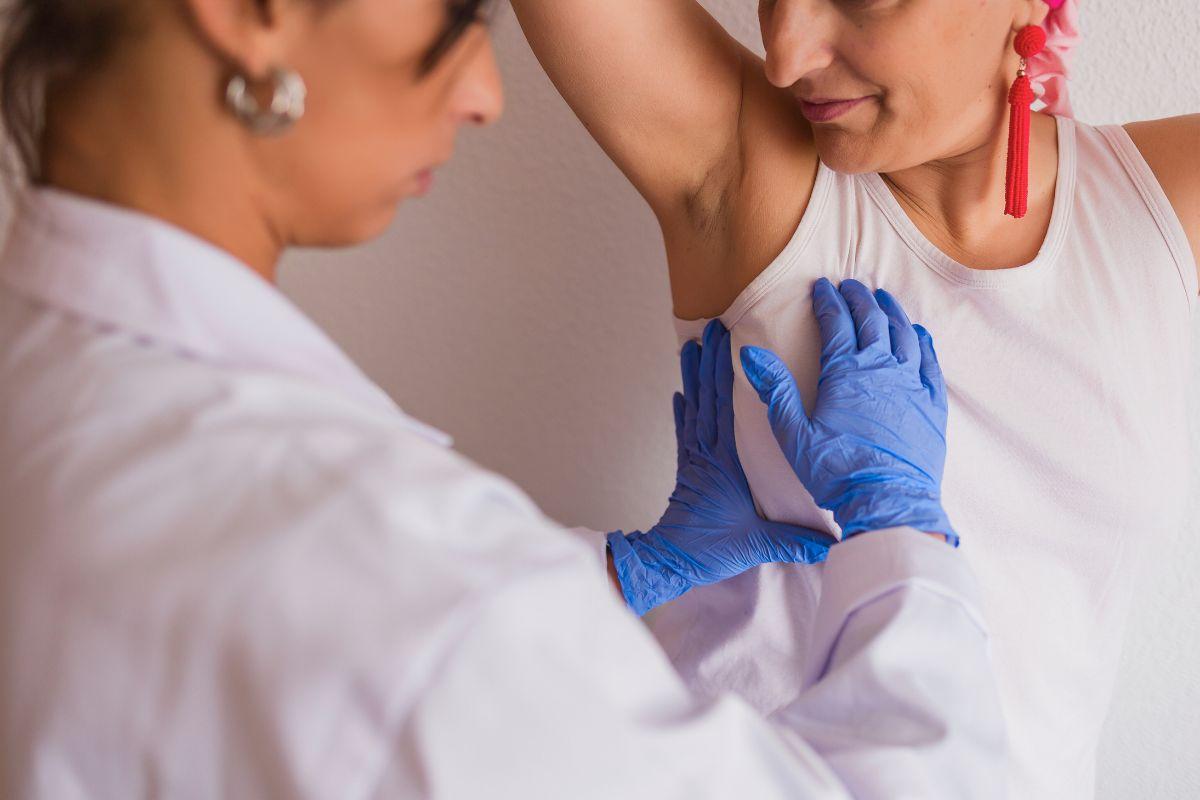
The first treatment option for stress urinary incontinence is pelvic floor muscle strengthening exercises supervised by a specialist pelvic floor physiotherapist. This can improve incontinence in 6 out of 10 women. Weight loss has also been shown to significantly improve stress urinary incontinence symptoms and topical oestrogen supplements can be applied to the vagina in post-menopausal women with good success.
Can it be helped with antibiotics?
In terms of medication, duloxetine, an anti-depressant, has also been found to be effective in improving symptoms of stress urinary incontinence in women. However, it does lead to side effects such as nausea and vomiting. It is generally only recommended for women who do not wish to undergo surgery or in women who have health problems that mean they are not suitable for surgery
What about surgery?
A number of surgical procedures exist for the treatment of stress urinary incontinence that has not improved with pelvic floor muscle exercises. The option that is best for you will depend on a number of factors, such as what you want and what the results of your detailed investigations show to be the main cause of your incontinence symptoms. It is therefore important to see a specialist who can discuss all these options with you. You both can then decide the best option for your specific case.
The various surgical options are?
- Sling procedures using synthetic materials (tension-free vaginal tape or transobturator tape). This is a relatively minor procedure with a short recovery time. A synthetic sling is placed under your water pipe (urethra) to provide support to your urethra when you cough or exercise, thereby stopping your incontinence. Incontinence improves in approximately 8 out of 10 women. However, a small number of women develop complications related to the tape. These can include chronic pain and erosion (damage to your water pipe or bladder by the tape)
- Sling procedures using natural tissue (autologous fascial slings). This is similar to the synthetic sling procedure but uses your own body tissue as the sling instead of synthetic material. The sling is made from the tissue that surrounds your abdomen muscles (rectus fascia). The surgery involves making a small bikini line cut in your lower abdomen. The recovery time is around six weeks and incontinence improves in approximately 8 out of 10 women. The risks of chronic pain or erosion are extremely rare but some women may find it harder to empty their bladder afterwards. These patients may need to pass a small tube into their bladder to empty it (self-catheterisation)
- Colposuspension. This is an open operation done through a bikini line cut in your lower abdomen. Stitches are placed either side of the bladder to provide extra support when you cough or exercise. Incontinence improves in approximately 8 out of 10 women and the recovery time is around six weeks
- Periurethral bulking agent injections. This involves injecting a bulking agent into your water pipe (urethra) using a telescope. The procedure takes 10 minutes and you can go home the same day. The risk of complications is low. However, repeat injections may be needed and success rates are lower than the other options